Corneal Transplants
What is a Corneal Transplant or Corneal Graft?
The cornea is the clear tissue that covers the front of the eye. It is the first point where light enters. The cornea must remain clear for vision to be sharp. The cornea is made up of five transparent layers.
A corneal transplant is used to replace corneal scarring from either trauma or infection, for diseases such as progressive keratoconus where the central cornea has become significantly thinner and inherited conditions such as Fuch’s dystrophy. It is replaced with healthy donor tissue.
Why is it done?
A cornea transplant is the best way to restore vision to a damaged cornea.
It often relieves pain.
Conditions that can be treated with a transplant-
- Fuch’s Endothelial Corneal Dystrophy- an inherited disease causing mistiness of the cornea
- Keratoconus- progressive where central cornea has become thin
- Bullous Keratopathy- swelling/ blisters at the front of the eye which are often painful
- Clouding of the cornea
- Corneal scarring caused through either injury or trauma
- Scarring from corneal ulcers caused by Herpes Zoster/ Keratitis
Types of Corneal Transplants
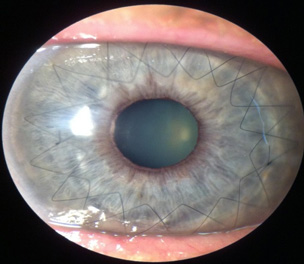
Penetrating Keratoplasty (full thickness 5 layers) PK:
This transplant involves removing all 5 layers of the cornea and replacing with donor tissue which is sutured into place. Cataract surgery is sometimes performed at the same time.
It is generally done as a day procedure with an overnight stay with local anaesthetic and sedation. The procedure can take anywhere from 60- 90 minutes.
Recovery generally is up to 18 months to achieve maximum recovery in vision. Sutures are normally removed after approximately 12 months due to the slow healing of the cornea.
Deep Anterior Lamellar Corneal Transplant (DALK):
This procedure is only replacing the front layers of the cornea with a transplant leaving the healthy back layer, known as the endothelium, in place. This procedure is often appropriate for patients where the disease process is only affecting the front portion of thecornea. Most commonly, this procedure is performed for keratoconus and corneal scars.
DSEK & DSAEK – Descemets’ Stripping Endothelial Keratoplasty
The diseased endothelial layer of the cornea is replaced rather than the full thickness. This is often used in patients suffering from Fuch’s Dystrophy. The main aim is to remove the minimal amount of tissue and replace it with healthy donor tissue, this often reduces swelling. It uses small incision surgery.
This surgery is performed as a day procedure with overnight stay under a local anaesthetic and sedation.
DSEK has a quicker recovery time compared to a full thickness transplant due to smaller incision which promotes better vision due to decreased astigmatism, lower risk of rejection due to less corneal tissue being used and quicker recover time of 3-6 months.
As with any transplant surgery there is the risk of rejection and there may a need for a re-do graft.
DMEK – Descemets Membrane Endothelial Keratoplaty
This is the newest technique used for partial thickness corneal transplants. Only the endothelial layer and the membrane holding the endothelial cells are replaced. The transplant in total is only about 20 micrometers thick.
It is a technique using small incision. The patient’s original cornea is left mostly intact; it replaced only the damaged corneal endothelial cells.
The main advantages include minimal invasive due to small incision, quicker visual recovery and a better chance of recovering 20/20 vision compared to PK and DSEK surgery.
This form of transplant is not suitable for all patients. This is due to the delicate nature of the donor cornea. The suitability of an individual for a particular type of corneal transplant will be assessed by your ophthalmologist.
Risks Associated With Corneal Transplant:
Cornea transplant is a relatively safe procedure however as with any surgery there are risks of complications.
- Corneal Transplant Rejection – symptoms often include loss of vision, increased pain and redness, light sensitivity which may require an increased frequency of eye drops of in some cases repeated surgery
- Increased risk of developing cataract
- Infection
- Increased pressure leading to glaucoma
- Loose stitches causing irritation
- Oedema ( swelling) of the cornea