Diabetic Retinopathy
What is Diabetic Retinopathy (DR)?
Diabetic retinopathy is a serious diabetic eye disease. It is the leading cause of preventable blindness in the working Australian population.
The tiny blood vessels located in light sensitive tissue in the back of the eye known as the retina are damaged by diabetes. If this condition is not monitored and managed, it may lead to blindness.
What are the risk factors for Diabetic Retinopathy (DR)?
People with either Diabetes Type 1 or 2 with a long history are at higher risk of developing DR. The other risk factors are:
- Uncontrolled blood sugar levels.
- Uncontrolled high blood pressure.
- Poorly controlled lipid levels.
- Smoking.
- Poor diet.
- Women who were diagnosed with gestational diabetes or polycystic ovary syndrome are at increased risk of developing type 2 diabetes. May develop DR later in life.
- Genetics can affect the onset, severity and speed of DR.
- Indigenous Australians and Torres Strait Islander Australians are more likely to develop diabetes compared to the rest of the Australian population. This increases their chance of DR
- Other groups at high risk are people of Middle Eastern and Asian populations and Pacific Islanders.
What are the symptoms of Diabetic Retinopathy?
During the early stages of this condition, people will usually not notice any visual symptoms. As the condition progresses and advances the following symptoms may occur;
- Straight lines appear distorted.
- Missing, or jumping letter/words when reading.
- Blurred vision.
- Dark, blurry, grey spots appear in the central vision.
- Floaters.
- Flashes of light.
- Sudden loss of vision.
People should not wait until symptoms present themselves before seeing an ophthalmologist.
Types of Diabetic Retinopathy
Non-proliferative diabetic retinopathy (NPDR)– This is also known as background diabetic retinopathy (BDR). There are three stages which are termed; mild, moderate and severe.
Damage occurs within the layers of the light sensitive area in the back of the eye known as the retina.
Some signs seen are;
- Microaneurysms (abnormal swelling of the tiny blood vessels).
- Blocked blood vessels causing poor blood supply to nourish the retina.
- Grow weak abnormal blood vessels (due to poor blood supply).
- Hard exudates (blood vessels leak out fatty deposits and cholesterol into the retina).
- Diabetic macular oedema (DME, swelling of the macula which is the area in the retina used for our central vision).
- Macular Ischaemia (loss of blood supply to the central vision of the retina).
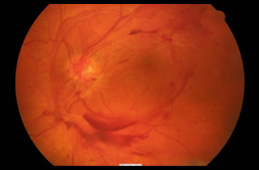
Proliferative diabetic retinopathy (PDR)
– This is the fourth and most advance stage of diabetic retinopathy. It will have signs of NPDR.
At this stage, this condition worsens and there is poor blood supply to the retina. Abnormal weak blood vessels grow to try and nourish the retina. These vessels can bleed without warning into the vitreous gel (Jelly like substance found in the eye back part of the eye).
The abnormal vessels can cause scarring and tension. This can cause the retina to wrinkle or retinal detachment.
How is Diabetic Retinopathy diagnosed?
Diabetic retinopathy is diagnosed by the ophthalmologist through a comprehensive eye examination using a special microscope called a slit lamp.
Pupil dilatation will be required to allow for a thorough evaluation of the macula, retina and optic nerve.
Other tests to expect are:
History taking: Evaluate potential risks and control of diabetes.
Vision testing: Assessing central vision.
Amsler Grid: A card with a grid to assess distortion or blurred spots.
OCT Scans (Optical Coherence Tomography: A non-invasive scan of the macula to identify retinal structural changes including fluid.
It also scans the optic nerve and allows for nerve fiber bundle layers to be analysed for any potential changes.Additional tests:
FFA (Fundus Fluorescein Angiography): Fluorescein dye is injected into the arm and photographs are taken of the retina.
This is to assess for leaking blood vessels, macula oedema, macular ischaemia and new abnormal vessels growing in the eye which can cause bleeding. This test takes about 15 minutes to do.
Management/Treatment
Diabetic retinopathy requires regular monitoring by the ophthalmologist. Appointments will depend on the treatment needed.
Regular monitoring and control of blood sugar levels are important as well eating a balance and diet and regular exercise. Lifestyle changes such as; reducing alcohol consumption and to stop smoking.
The ophthalmologist will work with your family doctor, dietician and endocrinologist to manage uncontrolled blood sugar, blood pressure and blood cholesterol levels.
There may be more than one of the following treatments needed to help control diabetic retinopathy.
Laser
There are two types of laser treatments. There is the focal laser and the pan-retinal photocoagulation (PRP) laser. Usually more than one PRP laser treatment is required.
Focal laser: Used to seal the leaking retinal blood vessels causing diabetic macular oedema (DME) and to also shrink the abnormal retinal vessels.
PRP laser: Used to treat proliferative diabetic retinopathy (PDR). Laser is applied into the peripheral retina to shrink blood vessels. It also stops the stimulation of abnormal blood vessel growth.
Intravitreal Injections
Currently intravitreal injections are the primary form of treatment for diabetic macula oedema (DME). Drugs such as Avastin and Lucentis are used to inject into the white part of the eye known as the sclera.
These are anti –VEGF (Vascular Endothelial Growth Factor) drugs. VEGF are proteins within the eye that trigger the growth of abnormal vessels and fluid accumulation within the retinal layers.
Avastin and Lucentis are used to treat this. Initially three courses of injections are given, normally four weeks apart.
The primary aims of these drugs are to dry out the fluid in the retina and gain some visual improvement.
Avastin (Bevacizumab): Is a non TGA (Therapeutic Good Administration) approved drug that has been used by ophthalmologist around the world for over 10 years. It has been proven to be quite effective.
Lucentis (Ranibizumab): Was originally approved by the TGA to treat ARMD (Age related macular degeneration). Recently it has been approved for use to treat diabetic macular oedema.
Eylea (Aflibercept): Is a TGA approved drug to treat ARMD. In the future it may be approved to treat diabetic macular oedema.
What are the risks/side effects of Intravitreal injection?
A patient may experience some irritation, grittiness and sandy sensation following the injection. The eye may water and usually settles down the next day. The antiseptic used to prepare the eye for the procedure may cause this sensation.
The ophthalmologist may prescribe their patients antibiotic eye drops or ointment after the injection.
As with any minor surgery procedure there is a small risk of complication such as infection of the eye. Usually this can be treated with medicated drops and injections.
Surgery
Vitrectomy: Is required to remove recurrent bleeding caused by the abnormal blood vessels. Blood and scar tissue is removed along with the vitreous gel (jelly in the eye between the front and back of the eye). Scar tissue can cause retinal detachment.
The vitreous gel is replaced with either salt solution, gas (avoid air travel for two months) or silicone oil (a second surgery may be needed to remove the silicon oil at a later date).
During this procedure or at a later date the natural lens of the eye is removed, as a cataract is likely to develop due to the silicon oil. This will allow for non-obstructed view for future examinations.
With surgery there is always risk of infection as well as failure to prevent further abnormal vessels bleeding. In some cases permanent vision loss can result.